US drug trial – cures all patients of rectal cancer with immunotherapy
In a hopeful incident, a drug trial in US cures all its patients of rectal cancer. With no radiation and chemotherapy these patients are cured only through immunotherapy
There are many incremental advances in science and technology which are impacting cancer patients and their families in a positive way. It can be a new drug or new technique of surgery either saving more lives or leading to faster recovery and reduced side-effects. Among the various treatments available for cancer patients especially in the curative setting, radiation therapy is an extremely important treatment. Approximately 50-60% of cancer patients need radiation therapy during their lifetime either as a single treatment or in combination of chemotherapy or surgery or both. Conventional radiation therapy most commonly involves use of X-rays and is usually given from outside the body and hence is referred to as “external beam radiation therapy”.
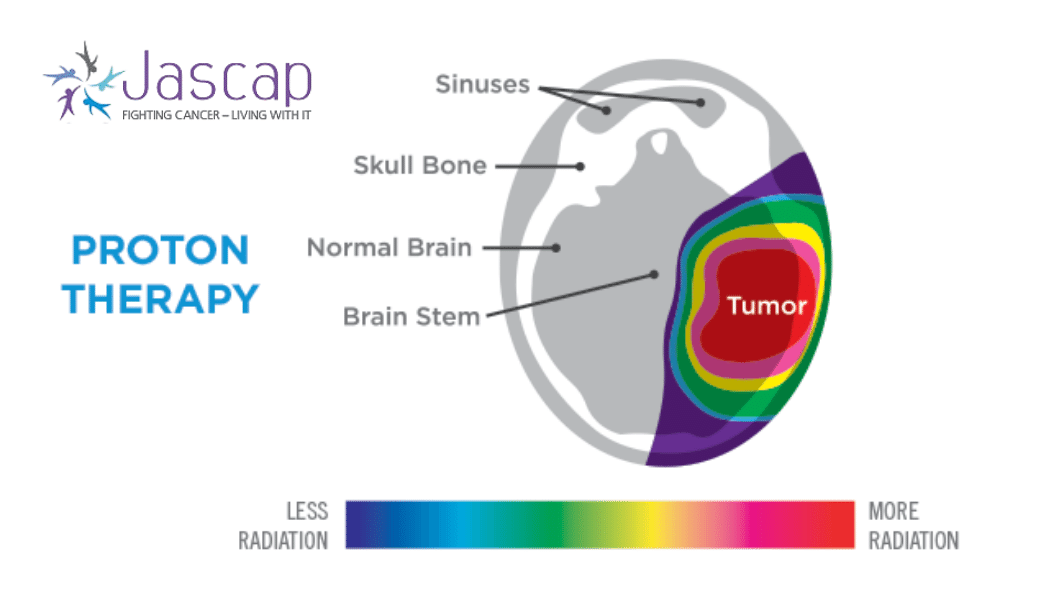
Radiation therapy along with the surgery for cancers is one of the oldest treatment available for cancer and has been discovered just before the beginning of the 19th century. Since then it has undergone several radical transformations to the current state where it is far more focused toward the tumors and therefore leads to lesser side-effects while eradicating the tumor. These advances in radiation therapy have been termed as “IMRT-intensity modulated radiotherapy” or “IGRT-image guided radiation therapy” or “volumetric modulated arc radiotherapy” and have been sometimes popularly known as “Helical Tomotherapy”, “Rapidarc” or “Cyberknife” after the brand or the company that manufactures the machines that deliver these treatments. Although all these techniques of radiation deliver intended radiation to the tumors, they also deliver mild to moderate doses to the adjacent structures which results in side-effects. Fortunately, radiation therapy unlike chemotherapy is a local treatment which results in local effects and local side-effects. These side-effects may be related to irradiation of heart, lungs, kidneys, bowel, urinary bladder, bones, salivary glands, oral cavity, mucosa over the head neck, brain, etc. depending on the site of radiation. One of the radically different approaches to radiation has been something called particle therapy or more commonly known as “Proton therapy”.
Proton therapy uses relatively heavier, positively charged high energy protons to treat tumors or cancers. Physically they are remarkably different compared to neutral X-rays which do not have a mass. Due to the physical difference, they stop after travelling finite distance within the body. That means by choosing appropriate energy of protons you can ensure that they stop within the tumor so that there would be literally no or “zero” radiation to structures beyond and around the tumor. This property of no exit dose of proton therapy can be exploited to deliver very high doses to the tumors without giving any radiation to adjacent structures which is physically impossible to achieve with conventional X-ray based radiation therapy. Biologically they are also more effective than X-rays and hence could be more effective in eradicating tumors compared to x-rays especially for certain relatively resistant (radio-resistant) tumors. However, proton therapy needs much larger infrastructure and is very resource intense to build and maintain making it relatively expensive compared to X-rays.
In the last 2 decades, proton therapy has also seen many incremental changes which has made proton therapy more efficient and safer. Although, proton therapy can be given to any patient who is likely to benefit with radiation therapy, it cannot be used for all due to its higher cost and limited access. Therefore, Proton therapy is considered standard for cancers or tumors in children/adolescents/young adults, tumors located near spine or base of skull, certain brain tumors and those patients requiring radiation for the second time. It is of a significant benefit in several cancers in the chest such as cancers of lung, food pipe or lymph nodes; cancers in head neck region, cancers in pelvis, etc. In all these patients, proton therapy can significantly minimize the probability of side-effects such as hearing loss, loss of vision, hormonal imbalance, infertility, sexual dysfunction, etc; and in some situations, even life-threatening side-effects such as cardiac malfunction, lung and liver damage could also be avoided.
Will proton therapy completely replace conventional radiation therapy? Probably not in the near future and the reasons are the cost and access. There is currently only one proton therapy centre in India (in Chennai) and one other is under construction (in Mumbai). The high cost of producing the proton beams will remain a major deterrent for rapid expansion of this technology. However, it is likely that there will be many more centres in the future and hopefully many more deserving patients would benefit from this engineering marvel.
It is very important that you understand the disease and the treatment involved.
JASCAP has books to help you understand PROTON THERAPY and fight it.
Books in 11 different languages can be found on
https://jascap.org/cancer-books-pdf/

In a hopeful incident, a drug trial in US cures all its patients of rectal cancer. With no radiation and chemotherapy these patients are cured only through immunotherapy

Tobacco is one of the most leading causes of cancer. It kills more than 8 million users every year. Risk of tobacco is increasing daily and it is important to understand how dangerous it is.

Dr Vikas – Times of India UP edition, March 06 2022

